Atopic Dermatitis and Eczema - many studies
Vitamin D Life - Atopic Dermatitus more likely if e-cigarette, passive smoke while pregnant or Caesarean
Atopic Dermatitis reduced if add Vitamin D - meta-analysis Nov 2024
Vitamin D Supplementation for Treating Atopic Dermatitis in Children and Adults: A Systematic Review and Meta-Analysis
Nutrients 2024, 16(23), 4128; https://doi.org/10.3390/nu16234128
by Amalie Ying Nielsen 1ORCID,Simon Høj 2ORCID,Simon Francis Thomsen 3ORCID andHowraman Meteran 4,5,6,*ORCID
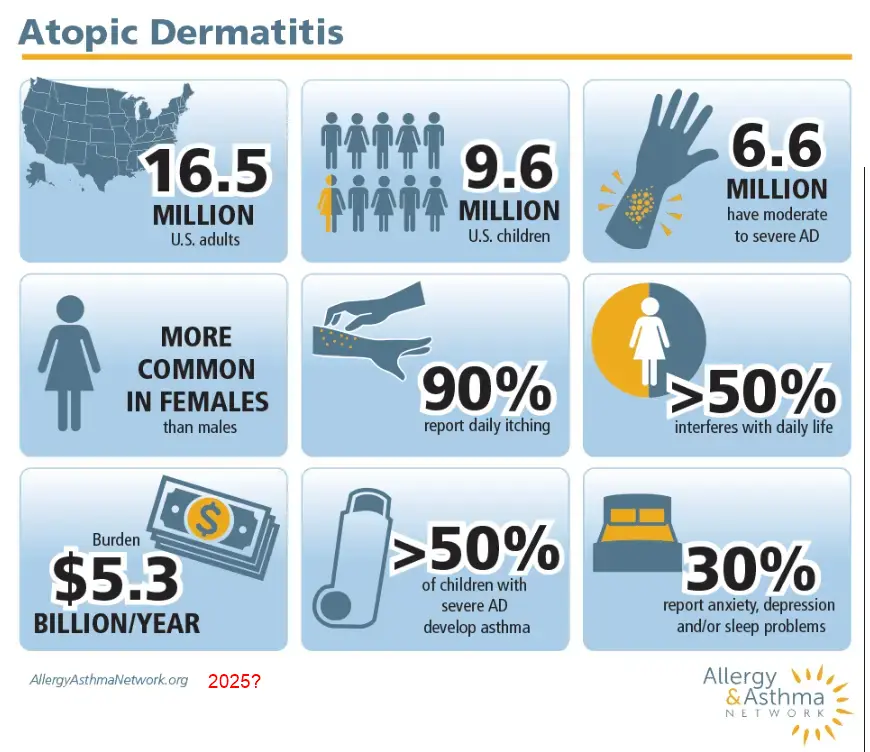
Background: Atopic dermatitis (AD) is a chronic inflammatory skin disease affecting up to 20% of children and 10% of adults worldwide. Current research suggests a correlation between serum vitamin D level and AD severity and that vitamin D supplementation could have a potential therapeutic effect on AD.
Objectives: To conduct a systematic review and meta-analysis of studies of vitamin D supplementation for disease improvement in children and adults with AD. Methods: PubMed, EMBASE, and Cochrane were searched from 19 April to 20 April 2024. We included randomized controlled trials (RCTs) of patients with AD comparing an intervention group with a control group. The risk of bias of the selected studies was assessed using the Cochrane risk-of-bias tool for randomized trials. All analyses were conducted in R (v4.1.2; R Core Team 2021).
Results: Eleven RCTs with 686 participants were included. The included trials had measured AD severity by using the SCOring Atopic Dermatitis (SCORAD) or the Eczema Area and Severity Index (EASI). Vitamin D supplementation significantly reduced AD severity compared with the control group (standardized mean difference = −0.41, 95% CI: −0.67 to −0.16, I2 = 58%, p < 0.01).
Conclusions: Vitamin D supplementation reduces AD severity in children and adults.
Larger-scale and longer-term studies are still needed to confirm this conclusion.
This study has been registered on PROSPERO (CRD42024535014).
📄 Download the PDF from Vitamin D Life
Food and mite allergies strongly associated with low vitamin D - April 2024
Vitamin D level is inversely related to allergen sensitization for risking atopic dermatitis in early childhood
World Allergy Organization Journal, Volume 17, Issue 4, April 2024, https://doi.org/10.1016/j.waojou.2024.100890
Chin-Hsuan Shen MD a b, Chun-Bing Chen MD c d, Meng-Han Chiang MSc e, Chieh-Ni Kuo BS b, Wen-Hung Chung MD, PhD c, Yin-Ku Lin MD, PhD f g, Chih-Yung Chiu MD, PhD e h
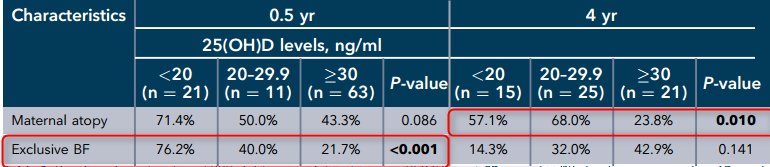
Subset of table with items with p <0.05
Background
There are few studies concerning the impact of serum vitamin D status on the risk of allergen sensitization and atopic dermatitis (AD) during early childhood.
Method
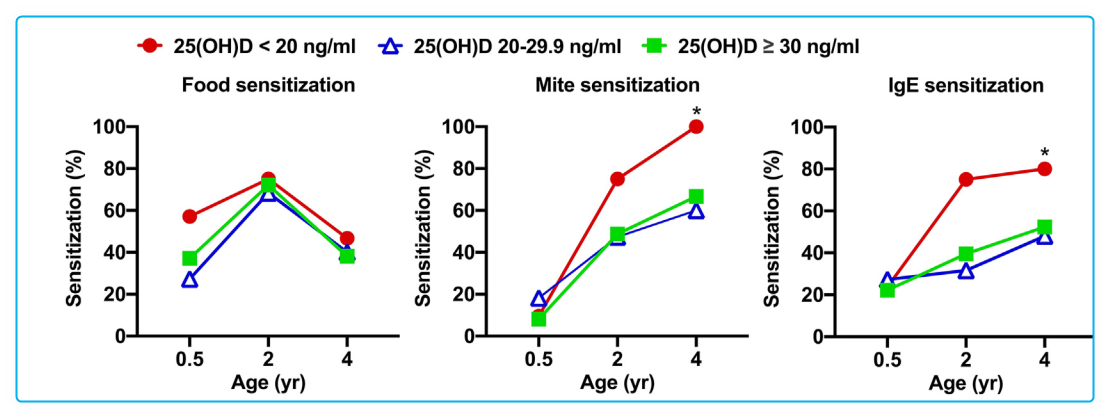
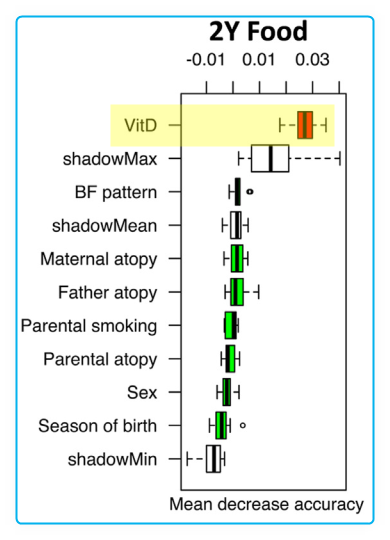
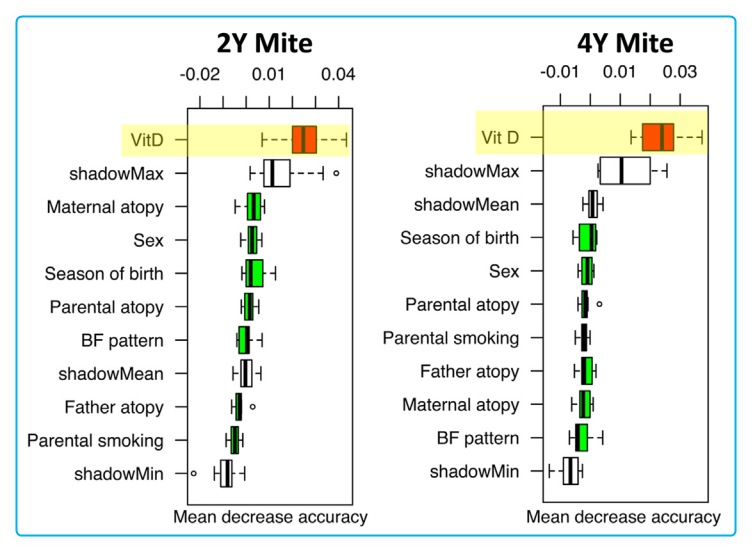
Children with AD and age-matched healthy controls (HC) were prospectively enrolled at age 0.5, 2, and 4 years. Serum 25-hydroxyvitamin D (25[OH]D) level was measured using Elecsys Vitamin D Total assay. The study utilized the ImmunoCAP assay to analyze specific IgE for food and inhalant allergens, along with total serum IgE levels. It explored the connection between vitamin D levels and allergen sensitization, as well as their influence on AD at different ages.
Results
A total of 222 children including 95 (59 AD and 36 HC), 66 (37 AD and 29 HC), and 61 (32 AD and 29 HC) children were classified at age 0.5, 2, and 4 years, respectively. In children with AD, there was a significantly lower vitamin D level at age 2 and 4, but a significantly higher prevalence of food and mite sensitization at all ages in comparison with HC (P < 0.001). Vitamin D level was found to be inversely related to the prevalence of allergen sensitization at age 4 (P < 0.05). However, vitamin D level appeared to have high importance for allergen sensitization at all ages and AD at age 2 and 4 years.
Conclusion
Vitamin D deficiency is strongly associated with heightened prevalence of allergen sensitization, potentially increasing the susceptibility to AD in early childhood.
📄 Download the PDF from Vitamin D Life
How to prevent Atopic Dermatitis (Eczema) in 2024: theory and evidence – April 2024
The Journal of Allergy and Clinical Immunology: In Practice (2024), doi: https://doi.org/10.1016/jjaip.2024.04.048.
Derek K. Chu, MD PhD, Jennifer J. Koplin, PhD, Tasnuva Ahmed, MBBS MPH, Nazmul Islam, MBBS MPH, Chia-Lun Chang, Msc,
Atopic dermatitis (AD) or eczema is a chronic inflammatory skin disease characterized by dry, itchy, and inflamed skin. We review emerging concepts and clinical evidence addressing the pathogenesis and prevention of atopic dermatitis.
We review several interventions ranging from skin barrier enhancement strategies;
probiotics,
prebiotics, and
synbiotics,
and conversely antimicrobial exposure;
vitamin D and omega fatty acid supplementation;
breastfeeding and hydrolyzed formula;
house dust mite avoidance and immunotherapy.
We appraise the available evidence base within the context of the GRADE approach. We also contextualize our findings in relation to concepts relating atopic dermatitis and individual-patient allergic life trajectories versus a linear concept of the atopic march and provide insights into future knowledge gaps and clinical trial design considerations that must be addressed in future research. Finally, we provide implementation considerations to detect population-level differences in AD risk. Major international efforts are required to provide definitive evidence regarding what works, and what does not, for preventing AD.
📄 Download the PDF from Vitamin D Life
Atopic Dermatitis: statistics, perhaps increased risk after vaccination - June 2025
"In VAERS, I found nearly 2,470 case reports of suspected vaccine-induced Eczema , 1,075 cases of Purpura, and 2,268 cases of Psoriasis."
Substack Hyperbaric Oxygen treats this and many other problems
Risk of Eczema increased 1.86 X after MMR Vaccination - 2003 Free PDF
COVID vaccination study found NO increase in Eczema - Nov 2022 Free PDF
Efficacy of vitamin D supplementation on the severity of atopic dermatitis in children: A systematic review and meta-analysis - Sept 2023
F1000Res. 2023 Sep 25:11:274. doi: 10.12688/f1000research.106957.2. eCollection 2022.
Afif Nurul Hidayati 1 2, Sawitri Sawitri 1, Desiana Widityaning Sari 1, Cita Rosita Sigit Prakoeswa 1, Diah Mira Indramaya 1, Damayanti Damayanti 1, Iskandar Zulkarnain 1, Irmadita Citrashanty 1, Yuri Widia 1, Sylvia Anggraeni 1

Deleted the one trial that used only 1,000 IU for only a single month
Background: Atopic Dermatitis (AD) is a common dermatosis in children, that includes skin architecture defects, immune dysregulation, and changes of skin flora. Several new drugs have been found to reduce the severity of AD. Vitamin D is one of the new therapies that is still controversial. The purpose of this research is to conclude the efficacy of vitamin D on atopic dermatitis severity in children aged 0-18 years old.
Methods: A systematic search was conducted on the PubMed, Cochrane, ProQuest, Google Scholar, Clinical Trial website, and university repositories including studies published from January 2010 through October 2020. We compared populations, intervention, study design, and outcomes. Statistical analysis was done with Review Manager 5.4.1. Results: Eight articles met eligibility and inclusion criteria, four articles provided complete data and were analysed. Not all studies demonstrated the efficacy of vitamin D but a meta-analysis of four studies of vitamin D supplementation vs placebo found a mean difference of -0.93 (95%CI -1.76, to -0.11, p<0.001) of patient outcome, but statistically, there was no difference in cure rate (risk ratio 1.46 (95%CI 0.72, to 2.97, p=0.008) in vitamin D supplementation groups compared to placebo groups.
Conclusions: Vitamin D supplementation in paediatric atopic dermatitis patients could offer improvement of disease severity but the recommended dose and duration of administration cannot be concluded yet.
📄 Download the PDF from Vitamin D Life
Worse Atopic Dermatitis is associated with lower vitamin D – Sept 2023
Evaluation of the Impact of Serum Vitamin D Levels on the Scoring Atopic Dermatitis Index in Pediatric Atopic Dermatitis
Children 2023,10, 1522. https://doi.org/10.3390/ children10091522
Fatih £igek ' and Mehmet Tolga Köle 2©
Department of Pediatric Allergy and Immunology, Kartal Dr. Lutfi Krrdar City Hospital, University of Health Sciences, Istanbul 34870, Turkey
Department of Pediatrics, Kartal Dr. Lutfi Kirdar City Hospital, University of Health Sciences, Istanbul 34870, Turkey; [email protected]
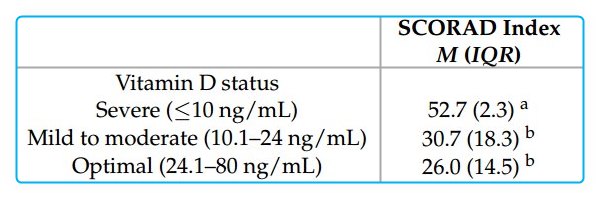
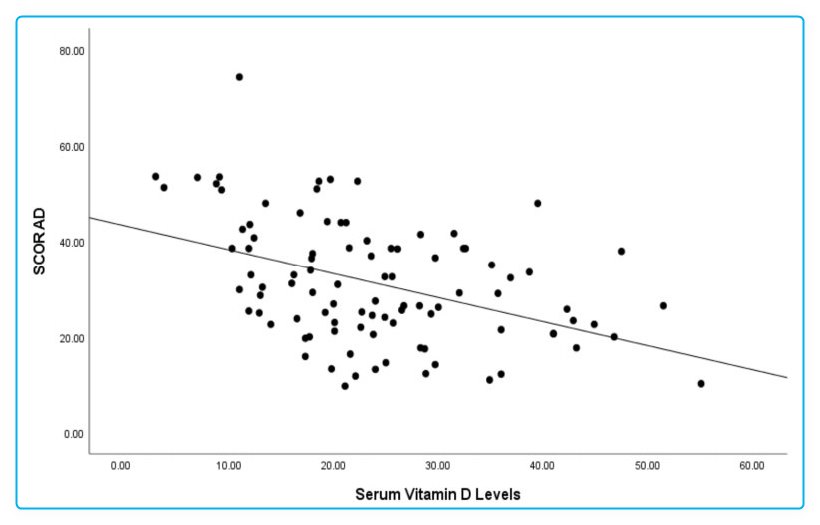
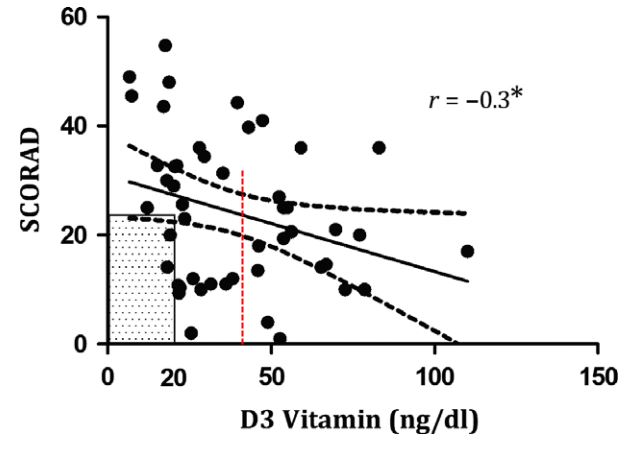
Atopic dermatitis (AD) is a chronic and recurrent inflammatory skin condition characterized by itching, eczematous plaques, and dry skin. Despite ongoing research, its exact cause remains elusive. In this study, we aimed to explore the factors that influence the severity of AD in children and assess the relationship between serum vitamin D levels and the disease's severity. We enrolled 96 AD patients in our investigation, evaluated their clinical condition using the Scoring Atopic Dermatitis (SCORAD) index, and compared them to a group of 90 healthy controls. Our analysis revealed that serum vitamin D levels and eosinophil counts significantly impacted the SCORAD index (p < 0.001). According to standardized regression coefficients, for each incremental unit in serum vitamin D levels, the SCORAD index exhibited a decrease of 0.449 units. Similarly, a one-unit increase in eosinophil count resulted in a 0.009 unit increase in the SCORAD index. It is worth noting that the influence of serum vitamin D levels on disease severity surpasses that of eosinophil counts and atopic conditions. In our patient cohort, we uncovered a negative correlation (r = -0.419, p < 0.001) between serum vitamin D levels and the SCORAD index. Our findings suggest that low serum vitamin D levels may have a more substantial impact on AD severity than atopic conditions and eosinophilia. Furthermore, we observed a negative association between the severity of AD and serum 25(OH)D3 levels.
📄 Download the PDF from Vitamin D Life
--
Atopic Dermatitis: 8 ng lower vitamin D - meta-analysis Aug 2022
Serum Vitamin D Level and Efficacy of Vitamin D Supplementation in Children with Atopic Dermatitis: A Systematic Review and Meta-analysis
Comput Math Methods Med . 2022 Jul 20;2022:9407888. doi: 10.1155/2022/9407888. eCollection 2022.
Hongbo Fu 1, Yanting Li 2, Huimin Huang 3, Dan Wang 3
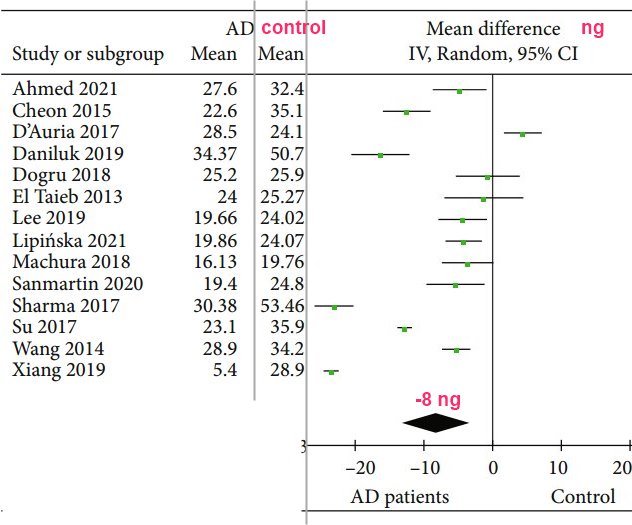
Background: The relationship between vitamin D and atopic dermatitis (AD) is controversial. This meta-analysis is aimed at exploring vitamin D level and its deficiency in pediatric AD and at evaluating the efficacy of vitamin D supplementation.
Methods: PubMed, Medline, Embase, Ovid, Cochrane Library, ISI Web of Science, and ClinicalTrials were searched. Binary variables and continuous variables were measured by odds ratio (OR) and mean difference (MD) with 95% confidence intervals, respectively. The modified Jadad scale, Newcastle-Ottawa Scale (NOS), and Cochrane's bias risk tools were used to evaluate study quality and the risk of bias of eligible studies, respectively.
Results: A total of 22 literature were included in the analysis. Serum 25 (OH) D level in pediatric AD patients was significantly lower than that of the control group with a combined MD value of -8.18 (95% CI: -13.15, -3.22). Patients with AD were more prone to develop vitamin D deficiency with a combined OR value of 2.17 (95% CI: 1.15, 4.11). According to the score of SCORAD, the level of serum 25 (OH) D level in patients with severe AD was significantly lower than that in patients with mild AD (combined MD = 9.23, 95% CI: 6.92, 11.55). Both self-control studies and randomized controlled trials showed improved SCORAD score and EASI score after vitamin D supplementation.
Conclusion: This meta-analysis showed lower serum 25 (OH) D level and increased risk of vitamin D deficiency in pediatric AD patients as compared with healthy controls. The serum 25 (OH) D level in severe AD patients was significantly lower than that in the mild AD patients. The SCORAD and EASI score improved after vitamin D supplementation, suggesting its beneficial effect to AD patients. At the same time, more homogeneous studies are needed to reduce confounding factors and further evaluate the impact of vitamin D treatment on the outcome of AD patients.
📄 Download the PDF from Vitamin D Life
Atopic Dermatitis 5X more likely if low Vitamin D - Aug 2019
Dose–response association between vitamin D deficiency and atopic dermatitis in children, and effect modification by gender: a case-control study
Amal Ahmed Mohamed, Eman Mohamed Salah Ahmed, Youssef M. K. Farag, Nermeen Ibrahim BedairORCID Icon, Nourelhuda Ahmed Nassar & Ayat Ibrahim Mohamed Ghanem
Background: Vitamin D is a regulatory factor for immunity and skin barrier functions. It is hypothesized to be linked to atopic dermatitis (AD) which is characterized by interaction between epidermal barrier dysfunction and dysregulation of skin immune functions.
Methods: One hundred AD patients and one hundred and one normal controls were collected from outpatient clinic based on their clinical condition, both had measurement of 25-hydroxyvitamin D [25(OH)D]. We assessed the relationship between 25(OH)D deficiency and AD prevalence using adjusted Poisson regression model.
Results: Serum 25(OH)D levels were significantly lower in cases than controls (mean 35.1 versus 22.6 ng/mL, p < .001). The unadjusted prevalence ratios (PRs) (95% CI) for AD for comparing participants with intermediate and deficient vitamin D levels to those with optimal levels were 3.11 (1.91, 5.06) and 4.77 (2.99, 7.60), respectively. The association did not materially change after adjusting for potential confounders. In the fully adjusted analysis stratified by gender, PRs for AD for comparing male participants with intermediate and deficient vitamin D levels to those with optimal levels were 3.38 (1.21, 9.40) and 5.20 (1.91, 14.13), respectively, whereas in the female participants were 1.32 (0.96, 1.83) and 1.49 (1.04, 2.14), respectively (p-interaction <.001).
Conclusion: In this case-control study in children, we found a statistically significant dose–response association between vitamin D deficiency and AD. We also observed a statistically significant effect modification of this association by gender. Further research is recommended to study this association longitudinally, and to examine whether treating vitamin D deficiency may potentially improve AD.
Atopic Dermatitis: treated by Vitamin D – Review of Micronutrients – March 2019
Micronutrients in Atopic Dermatitis: A Systematic Review
J Altern Complement Med. 2019 Mar 26. doi: 10.1089/acm.2018.0363.
Vaughn AR1, Foolad N2, Maarouf M3, Tran KA3, Shi VY4.
1 Department of Dermatology, University of California-Davis, Sacramento, CA.
2 School of Medicine, University of California-Davis, Sacramento, CA.
3 College of Medicine, University of Arizona-Tucson, Tucson, AZ.
4 Division of Dermatology, Department of Medicine, University of Arizona-Tucson, Tucson, AZ.
OBJECTIVE:
The pathophysiology of atopic dermatitis (AD) involves a complex interplay between immune system dysfunction, genetics, and environmental factors. It is well known that nutritional status is essential to a proper functioning immune system, leading to a highly debated question regarding the role of dietary factors in the pathogenesis of AD. Food allergies and elimination diets have been broadly studied in atopy; however, less consideration has been given to how vitamins, minerals, and other micronutrients influence the risk for AD and severity of symptoms. This systematic review discusses evidence on how various micronutrients, including vitamins (C, E, and D) and trace minerals (zinc, selenium, iron, copper, magnesium, and strontium) are associated with AD, and how supplementation influence disease severity.
DESIGN:
A systematic search was conducted to identify the role that oral micronutrients have on AD. The authors reviewed 49 studies herein.
RESULTS:
While there are weak associations between vitamins C or E and AD, there is sufficient evidence to suggest that vitamin D supplementation provides benefit in AD patients. Deficiency of selenium and zinc may exacerbate AD . Current reports are not sufficient to confidently discern the role of other vitamins and trace minerals on AD.
CONCLUSIONS:
Though oral micronutrients may play a role in AD, the current literature is limited, and there is a need for more comprehensive randomized controlled trials (RCTs) to truly decipher the role between oral micronutrients and AD.
Atopic dermatitis treatment needs more than 5,000 IU of Vitamin D – RCT Sept 2018
Oral vitamin D3 5000 IU/day as an adjuvant in the treatment of atopic dermatitis: a randomized control trial
International Journal of Dermatology 20 September 2018 https://doi.org/10.1111/ijd.14220
Karen Sánchez‐Armendáriz MD Ana García‐Gil MD Cesar A. Romero MD José Contreras‐Ruiz MD Marcia Karam‐Orante MD
PDF is available free at Sci-Hub 10.1111/ijd.14220
Background:Vitamin D has immunomodulatory effects both in the innate and adaptive immune systems, and there is growing scientific evidence demonstrating its relevance in inflammatory processes such as AD.
Hypothesis: If vitamin D3 promotes the skin immune system, then it should improve the response to treatment of patients with AD.
Methods
A randomized, double‐blind placebo‐controlled clinical trial was conducted, which included 65 patients with AD according to Hanifin–Rajka criteria and the severity scale (SCORAD). The patients were divided into two groups to receive either vitamin D3 5000 IU/day (n = 33) or placebo (n = 32), plus baseline therapy (topical steroid, soap substitute, and emollient) during 3 months.
Results
Fifty‐eight of the 65 enrolled subjects were included in the analysis. At the end of the intervention, the treated group achieved higher levels of 25(OH)D (P < 0.001). At week 12, those patients who registered serum levels of 25(OH)D ≥20 ng/ml, regardless of whether or not they had received supplementation, showed a lower SCORAD compared to those with levels <20 ng/ml (P < 0.001). Eighty percent of the patients with serum levels <20 ng/ml (n = 9) had moderate–severe AD despite standard treatment. Vitamin D levels ≥20 ng/ml associated with baseline therapy strongly favored remission of atopic dermatitis (P = 0.03). No significant differences were found between patients with serum levels of ≥20 ng/ml vs. ≥30 ng/ml.
Conclusions: Reaching serum levels of 25(OH)D > 20 ng/ml in conjunction with standard therapy is sufficient to achieve a reduction in severity (SCORAD) in patients with AD.
Atopic Dermatitis reduced by 5,000 IU of Vitamin D for 12 weeks – RCT Dec 2018
Oral vitamin D3 5000 IU/day as an adjuvant in the treatment of atopic dermatitis: a randomized control trial.
Int J Dermatol. 2018 Dec;57(12):1516-1520. doi: 10.1111/ijd.14220. Epub 2018 Sep 20.
Sánchez-Armendáriz K1, García-Gil A1, Romero CA2, Contreras-Ruiz J1, Karam-Orante M1, Balcazar-Antonio D3, Domínguez-Cherit J4.
BACKGROUND: Vitamin D has immunomodulatory effects both in the innate and adaptive immune systems, and there is growing scientific evidence demonstrating its relevance in inflammatory processes such as AD.
HYPOTHESIS: If vitamin D3 promotes the skin immune system, then it should improve the response to treatment of patients with AD.
METHODS:
A randomized, double-blind placebo-controlled clinical trial was conducted, which included 65 patients with AD according to Hanifin-Rajka criteria and the severity scale (SCORAD). The patients were divided into two groups to receive either vitamin D3 5000 IU/day (n = 33) or placebo (n = 32), plus baseline therapy (topical steroid, soap substitute, and emollient) during 3 months.
RESULTS:
Fifty-eight of the 65 enrolled subjects were included in the analysis. At the end of the intervention, the treated group achieved higher levels of 25(OH)D (P < 0.001). At week 12, those patients who registered serum levels of 25(OH)D ≥20 ng/ml, regardless of whether or not they had received supplementation, showed a lower SCORAD compared to those with levels <20 ng/ml (P < 0.001). Eighty percent of the patients with serum levels <20 ng/ml (n = 9) had moderate-severe AD despite standard treatment. Vitamin D levels ≥20 ng/ml associated with baseline therapy strongly favored remission of atopic dermatitis (P = 0.03). No significant differences were found between patients with serum levels of ≥20 ng/ml vs. ≥30 ng/ml.
CONCLUSIONS: Reaching serum levels of 25(OH)D > 20 ng/ml in conjunction with standard therapy is sufficient to achieve a reduction in severity (SCORAD) in patients with AD.
Increased risk of AD, etc if poor vitamin D Receptor or CYP24A1 gene - June 2023
Association Between VDR and CYP24A1 Polymorphisms, Atopic Dermatitis, and Biochemical Lipid and Vitamin D Profiles in Spanish Population: Case-Control Study
JMIR Dermatol. 2023 Jun 27;6:e39567. doi: 10.2196/39567.
Ricardo González-Tarancón 1, Nuria Goñi-Ros 1, Elvira Salvador-Rupérez 1, Ángela Hernández-Martín 2, Silvia Izquierdo-Álvarez 1, José Puzo-Foncillas 3, Yolanda Gilaberte-Calzada 4
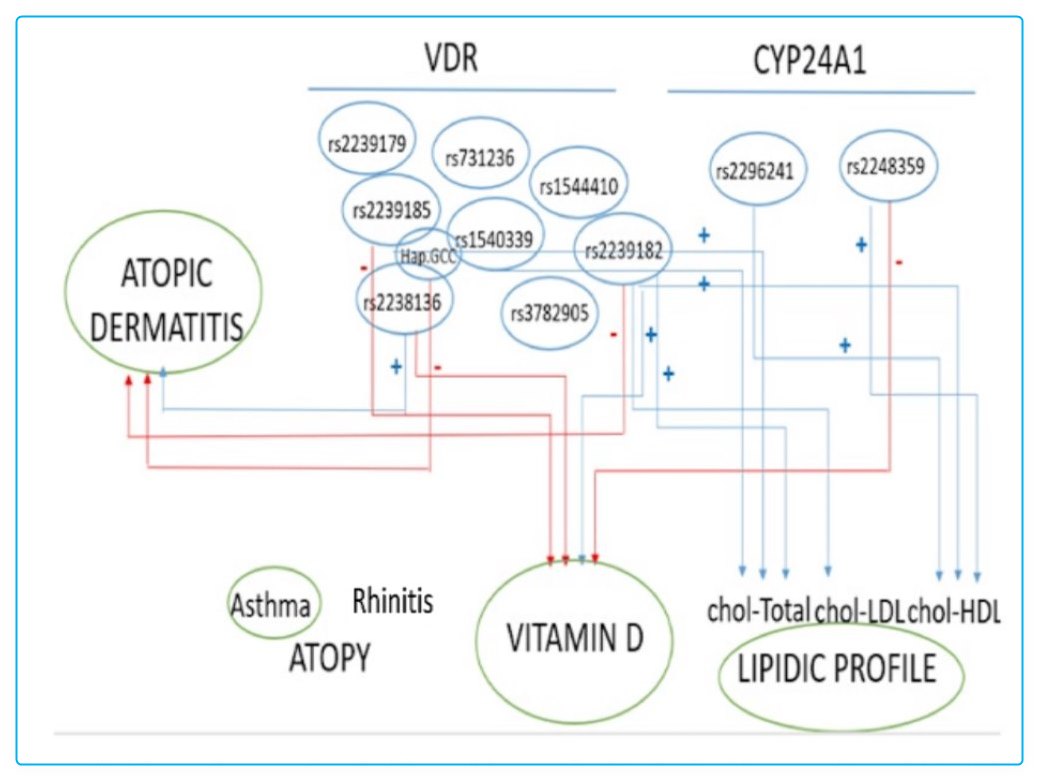
Background: Atopic dermatitis (AD) is the most prevalent inflammatory skin disorder, characterized by impaired epidermal barrier function and an altered immune response, both of which are influenced by vitamin D deficiency. Single-nucleotide polymorphisms (SNPs) in VDR and CYP24A1 have been previously associated with AD.
Objective: We sought to characterize the associations between the VDR and CYP24A1 polymorphisms and the vitamin D and lipid biochemical profile in children diagnosed with AD.
Methods: A total of 246 participants (143 patients with AD and 103 healthy controls) were enrolled in this study. Genotyping for polymorphisms in VDR (rs2239185, rs1544410, rs7975232, rs2238136, rs3782905, rs2239179, rs1540339, rs2107301, rs2239182, and rs731236) and CYP24A1 (rs2248359 and rs2296241) was performed by allele-specific polymerase chain reaction using integrated fluidic circuit technology. Serum levels of calcium, phosphorus, and vitamin D were measured, and the biochemical lipid profile was determined.
Results: Among VDR SNPs, rs2239182 exerted a protective effect against the development of AD, whereas rs2238136 was identified as a risk factor for AD. The GCC haplotype (rs2239185-G, rs1540339-C, and rs2238136-C) appeared to protect against the development of AD. rs2239182-CC was associated with higher 25(OH)D concentrations, whereas rs2238136-TT, rs2239185-GA, and rs2248359-TT were present in a large proportion of patients with serum vitamin D deficiency. rs2239185-AA, rs2239182-CC, and rs1540339-CC were associated with higher serum total cholesterol; rs2239182-TT was associated with lower low-density lipoprotein cholesterol; and rs2239182-TC with lower high-density lipoprotein cholesterol. Both CYP24A1 SNPs (rs2296241-AA and rs2248359-TT) were associated with higher high-density lipoprotein cholesterol levels.
Conclusions: The VDR SNP rs2238136 is a risk factor for AD and other SNPs in VDR and CYP24A1, which may lead to alterations in biochemical parameters that influence the risk of AD. Our findings highlight the complex genetic basis to AD and indicate that interrelationships between different genetic factors can lead to alterations in vitamin D metabolism or lipid profiles, which in turn may influence the development of AD.
📄 Download the PDF from Vitamin D Life
Vitamin D fights many skin diseases, topical form might be best
- Topical vitamin D is especially useful for Skin diseases
- - as vitamin D is focused on the skin problem, rather than the whole body
Randomized controlled trial using vitamins E and D supplementation in atopic dermatitis - July 2011
J Dermatolog Treat. 2011 Jun;22(3):144-50
Javanbakht MH, Keshavarz SA, Djalali M, Siassi F, Eshraghian MR, Firooz A, Seirafi H, Ehsani AH, Chamari M, Mirshafiey A.
Department of Nutrition and Biochemistry, Faculty of Public Health, Tehran University of Medical Sciences, Tehran, Iran.
BACKGROUND: Atopic dermatitis is a chronically relapsing, highly pruritic and inflammatory skin disease. This study was done to assess the effects of vitamins D and E supplementation on the clinical manifestation of atopic dermatitis.
METHODS: Forty-five atopic dermatitis patients were included in a randomized, double-blind, placebo-controlled trial. They were randomly divided into four groups and treated for 60 days: group P (n = 11), vitamins D and E placebos; group D (n = 12), 1600 IU vitamin D(3) plus vitamin E placebo; group E (n = 11), 600 IU synthetic all-rac-?-tocopherol plus vitamin D placebo; and group DE (n = 11), 1600 IU vitamin D(3) plus 600 IU synthetic all-rac-?-tocopherol. Serum 25(OH) vitamin D and plasma ?-tocopherol were determined before and after the trial. The clinical improvement was evaluated with SCORing Atopic Dermatitis (SCORAD). Data were analyzed by analysis of variance (ANOVA) and Kruskal-Wallis tests.
RESULTS: SCORAD was reduced after 60 days in groups D, E and DE by 34.8%, 35.7% and 64.3%, respectively (p = 0.004). Objective SCORAD also showed significant improvement. There was a positive correlation between SCORAD and intensity, objective, subjective and extent (p < 0.001). We found a significant negative association between plasma ?-tocopherol and SCORAD, intensity, objective and extent (p = 0.02).
CONCLUSION: This study supports the contributing and beneficial effects of vitamins D and E in the treatment of atopic dermatitis.
18+ Vitamin D Life pages with ATOPIC or ECZEMA in title
This list is automatically updated
{LIST()}
What is the difference between atopic dermatitis and eczema?
Eczema is used as a general term for many types of skin inflammation (dermatitis) and allergic-type skin rashes. There are different types of eczema, like allergic, contact, irritant, and nummular eczema. Several other forms have very similar symptoms. The diverse types of eczema are listed and briefly described below. Atopic dermatitis is typically a more specific set of three associated conditions occurring in the same person including eczema, allergies, and asthma. Not every component has to be present at the same time, but usually these patients are prone to all of these three related conditions.
Types of eczema
Contact eczema: a localized reaction that includes redness, itching, and burning where the skin has come into contact with an allergen (an allergy-causing substance) or with an irritant such as an irritating acid, a cleaning agent, or other chemical
Allergic contact eczema: a red, itchy, weepy reaction where the skin has come into contact with a substance that the immune system recognizes as foreign, such as poison ivy or certain preservatives in creams and lotions like Neosporin or Bacitracin
Seborrheic eczema (also called seborrheic dermatitis or seborrhea): is a very common form of mild skin inflammation of unknown cause that presents as yellowish, oily, scaly patches of skin on the scalp, face, ears, and occasionally other parts of the body. Often this is also called dandruff in adults or "cradle cap" in infants.
Nummular eczema: coin-shaped (round), isolated patches of irritated skin -- most commonly on the arms, back, buttocks, and lower legs -- that may be crusted, scaling, and extremely itchy
Neurodermatitis: a very particular type of dermatitis where the person frequently picks at their skin, causing rashes. The underling cause may be a sensitivity or irritation which sets off a cascade of repeated itching and scratching cycles. It may be seen as scratch marks and pick marks on the skin. Sometimes scaly patches of skin on the head, lower legs, wrists, or forearms caused by a localized itch (such as an insect bite) may become intensely irritated when scratched.
Stasis dermatitis: a skin irritation on the lower legs, generally related to circulatory problems and congestion of the leg veins. It may have a darker pigmentation, light-brown, or purplish-red discoloration from the congestion and back up of the blood in the leg veins. It's sometimes seen more in legs with varicose veins.
Seborrheic Dermatitis 4.2X more likely if <30 ng of Vitamin D - Feb 2021
Serum Levels of 25-Hydroxyvitamin D in Patients with Seborrheic Dermatitis: A Case-Control Study
Dermatol Res Pract . 2021 Feb 20;2021:6623271. doi: 10.1155/2021/6623271
Siavash Rahimi 1, Negar Nemati 1, Seyedeh Sareh Shafaei-Tonekaboni 1
Several autoimmune papulosquamous skin conditions such as psoriasis, systemic lupus erythematous, and lichen planus have been associated with vitamin D deficiency or correlated with serum vitamin D level. This study was aimed at comparing the 25-hydroxyvitamin D (25(OH)D) status in patients with facial or scalp seborrheic dermatitis with healthy subjects. This case-control study included 289 patients (118 with psoriasis and 171 sex- and age-matched control subjects) from the outpatient clinic of two hospital dermatology departments in the west of Mazandaran province, Iran. All patients and control subjects were studied during one season to avoid seasonal variations in vitamin D levels. Serum mean ± standard deviation of 25(OH)D levels were significantly lower in seborrheic dermatitis patients than in control subjects (20.71 ± 8.16 vs. 23.91 ± 7.78, P = 0.007).
Serum 25(OH)D levels were negatively associated with the risk of developing seborrheic dermatitis (odds ratio (OR): 0.898, 95% confidence interval (Cl): 0.840-0.960, P = 0.002).
Also, vitamin D under 30 ng/ml was associated with OR: 4.22 (95% Cl: 1.077-16.534, P = 0.039) for seborrheic dermatitis. The severity of scalp disease was significantly associated with serum 25(OH)D level (P = 0.003). Cases with severe scalp scores had significantly lower serum 25(OH)D level compared to moderate OR score (P = 0.036). A similar trend was not seen in the facial disease. The 25(OH)D values are significantly lower in seborrheic dermatitis patients than in healthy subjects. Furthermore, the scalp disease severity was associated with lower serum 25(OH)D level. Our results may suggest that vitamin D may play a role in the pathogenesis of seborrheic dermatitis.
📄 Download the PDF from Vitamin D Life
See also web
Eczema and Dermatitis Everwell - overview, probably nothing about Vitamin D
Pubmed query "atopic dermatitis." "vitamin d" 402 items March 2024
Correlation of Vitamin D3 Levels and SCORAD Index in Atopic Dermatits: A Case Control Study. Julu 2017
- The worse the AD, the lower the Level of vitamin D. (nmol/L) free PDF online
- None (controls) = 53, Mild = 33, Moderate = 31.5, Severe = 21
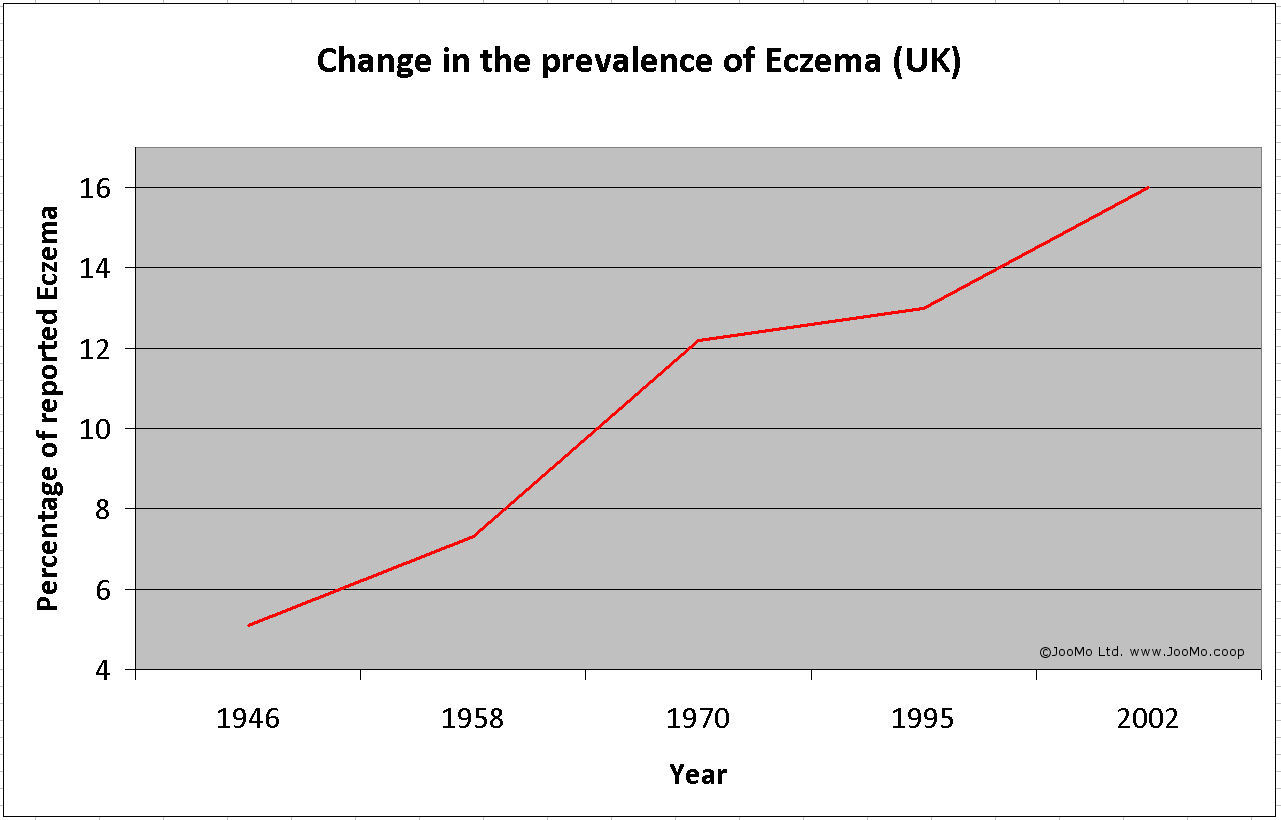
- Change in the prevalence of Eczema since the 2nd World War UK published 2012: has the following chart
Typical Eczema sites on body, scratching - images from web


